Coffee Secrets Gift Ideas
Coffee Secrets Gift Ideas is curated all seasons and occasions Gift Ideas Online Store, Holiday Gift Guide, Books, Bracelets, Calculators, Data Storage, Drone with Camera, Headphones, Luxury Watches, Bikes and Scooters, Safes and Lockboxes, Sleep Monitors, VR Headsets, Wireless Cellphone Chargers and more
Best Sellers by Coffee Secrets Gift Ideas
-
 Premium Poker Table for 8 Players with 8 Chairs and Additional Mat$2,399.99
Premium Poker Table for 8 Players with 8 Chairs and Additional Mat$2,399.99 -
 Drone Remote Controller Bike Mount for DJI$20.99Rated 4.75 out of 5 based on 4 customer ratings
Drone Remote Controller Bike Mount for DJI$20.99Rated 4.75 out of 5 based on 4 customer ratings -
Sale Product on sale
 Toilet Poop Stool Squatty Potty
Toilet Poop Stool Squatty Potty$16.99Original price was: $16.99.$16.59Current price is: $16.59.Rated 4.75 out of 5 based on 4 customer ratings -
 Driver Side Power Master Window Switch$25.68Rated 4.00 out of 5 based on 4 customer ratings
Driver Side Power Master Window Switch$25.68Rated 4.00 out of 5 based on 4 customer ratings -
Sale Product on sale
 Jump Starter 2000A Peak Portable Battery
Jump Starter 2000A Peak Portable Battery$67.00Original price was: $67.00.$53.99Current price is: $53.99. -
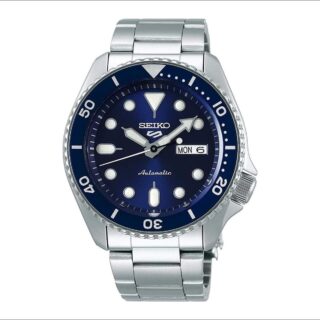
 SEIKO SRPD51 5 Sports Men’s Watch$229.90Rated 4.89 out of 5 based on 9 customer ratings
SEIKO SRPD51 5 Sports Men’s Watch$229.90Rated 4.89 out of 5 based on 9 customer ratings -
 Dr. Scholl’s Time Off Sneaker$69.99Rated 4.56 out of 5 based on 9 customer ratings
Dr. Scholl’s Time Off Sneaker$69.99Rated 4.56 out of 5 based on 9 customer ratings -
 BOGG BAG Original X Large Waterproof$90.00Rated 5.00 out of 5 based on 9 customer ratings
BOGG BAG Original X Large Waterproof$90.00Rated 5.00 out of 5 based on 9 customer ratings -
 Portable Grill Weber Q1200$237.75Rated 4.89 out of 5 based on 9 customer ratings
Portable Grill Weber Q1200$237.75Rated 4.89 out of 5 based on 9 customer ratings -
 Instant Print Camera for Kids$33.99Rated 4.78 out of 5 based on 9 customer ratings
Instant Print Camera for Kids$33.99Rated 4.78 out of 5 based on 9 customer ratings -
 All Seasons Plus Size Anorak Jacket$79.31Rated 4.56 out of 5 based on 9 customer ratings
All Seasons Plus Size Anorak Jacket$79.31Rated 4.56 out of 5 based on 9 customer ratings -
 Hands Free Dog Leash with Zipper Pouch$21.99Rated 4.89 out of 5 based on 9 customer ratings
Hands Free Dog Leash with Zipper Pouch$21.99Rated 4.89 out of 5 based on 9 customer ratings -
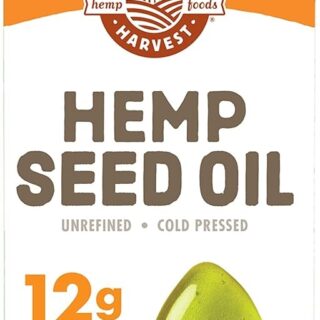
 Hemp Oil Cold Pressed$8.81Rated 4.86 out of 5 based on 7 customer ratings
Hemp Oil Cold Pressed$8.81Rated 4.86 out of 5 based on 7 customer ratings -
 Vintage Espresso Coffee Machine$301.59
Vintage Espresso Coffee Machine$301.59 -
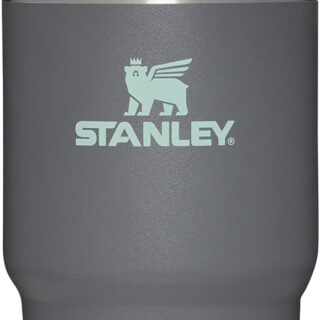
 Stanley Quencher H2.0$45.00Rated 5.00 out of 5 based on 9 customer ratings
Stanley Quencher H2.0$45.00Rated 5.00 out of 5 based on 9 customer ratings -
 Xiaomi Mi Band 7 Activity Tracker$45.96Rated 4.57 out of 5 based on 7 customer ratings
Xiaomi Mi Band 7 Activity Tracker$45.96Rated 4.57 out of 5 based on 7 customer ratings
-
Sale Product on sale
 Canon EOS 2000D Rebel T7 DSLR Camera
Canon EOS 2000D Rebel T7 DSLR Camera$649.00Original price was: $649.00.$429.95Current price is: $429.95. -
 Meta Quest 3 Bundle$499.99
Meta Quest 3 Bundle$499.99 -
 Xiaomi Mi Band 7 Activity Tracker$45.96Rated 4.57 out of 5 based on 7 customer ratings
Xiaomi Mi Band 7 Activity Tracker$45.96Rated 4.57 out of 5 based on 7 customer ratings -
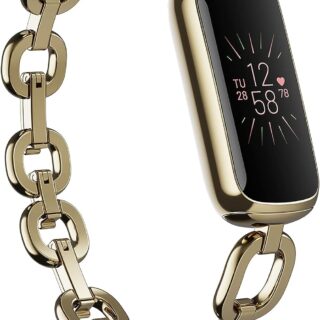
 Fitbit Luxe Fitness and Wellness Tracker$116.00Rated 4.22 out of 5 based on 9 customer ratings
Fitbit Luxe Fitness and Wellness Tracker$116.00Rated 4.22 out of 5 based on 9 customer ratings -
 Sleep Tracking Pad$129.95Rated 4.22 out of 5 based on 9 customer ratings
Sleep Tracking Pad$129.95Rated 4.22 out of 5 based on 9 customer ratings -
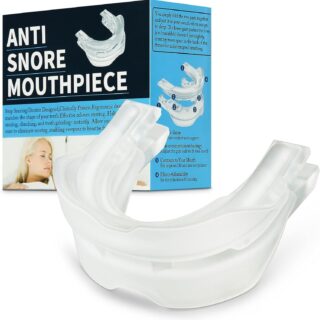
 Anti Snoring Mouthpiece$39.99Rated 4.86 out of 5 based on 7 customer ratings
Anti Snoring Mouthpiece$39.99Rated 4.86 out of 5 based on 7 customer ratings -
 Set of Nose Vents$14.96Rated 4.11 out of 5 based on 9 customer ratings
Set of Nose Vents$14.96Rated 4.11 out of 5 based on 9 customer ratings -
 Navage Nasal Irrigation Essentials Bundle$109.95Rated 4.67 out of 5 based on 9 customer ratings
Navage Nasal Irrigation Essentials Bundle$109.95Rated 4.67 out of 5 based on 9 customer ratings -
 Wearable Pulse Oximeter$159.99Rated 4.56 out of 5 based on 9 customer ratings
Wearable Pulse Oximeter$159.99Rated 4.56 out of 5 based on 9 customer ratings -
 Wireless Upper Arm Blood Pressure Monitor$142.00Rated 4.83 out of 5 based on 6 customer ratings
Wireless Upper Arm Blood Pressure Monitor$142.00Rated 4.83 out of 5 based on 6 customer ratings -
 Personal EKG Monitor$0.00Rated 4.13 out of 5 based on 8 customer ratings
Personal EKG Monitor$0.00Rated 4.13 out of 5 based on 8 customer ratings -
 Personal EKG Monitor$129.00Rated 4.44 out of 5 based on 9 customer ratings
Personal EKG Monitor$129.00Rated 4.44 out of 5 based on 9 customer ratings -
 Portable 5TB External Hard Drive HDD$109.99Rated 4.56 out of 5 based on 9 customer ratings
Portable 5TB External Hard Drive HDD$109.99Rated 4.56 out of 5 based on 9 customer ratings -
 20TB Desktop External Hard Drive$345.94Rated 4.78 out of 5 based on 9 customer ratings
20TB Desktop External Hard Drive$345.94Rated 4.78 out of 5 based on 9 customer ratings -
 WD 5TB Portable External Hard Drive HDD$129.99Rated 4.78 out of 5 based on 9 customer ratings
WD 5TB Portable External Hard Drive HDD$129.99Rated 4.78 out of 5 based on 9 customer ratings -
 XREAL Air AR Glasses$429.00Rated 3.67 out of 5 based on 3 customer ratings
XREAL Air AR Glasses$429.00Rated 3.67 out of 5 based on 3 customer ratings -
 VR Goggles Headset for Smartphone$33.99Rated 4.67 out of 5 based on 3 customer ratings
VR Goggles Headset for Smartphone$33.99Rated 4.67 out of 5 based on 3 customer ratings -
 HTC VIVE Pro 2 Virtual Reality System$1,399.00Rated 4.14 out of 5 based on 7 customer ratings
HTC VIVE Pro 2 Virtual Reality System$1,399.00Rated 4.14 out of 5 based on 7 customer ratings
Discover more from Coffee Secrets Gift Ideas
Subscribe to get the latest posts to your email.